NAB client Zenith Energy’s innovation is helping decarbonise the mining sector through providing efficient hybrid generation solutions in remote areas.


What do your patients think about vital issues like chronic illness prevention and mental health? This survey uncovers some surprising facts.
What aren’t your patients telling you? NAB’s new Consumer Health Survey lifts the lid on some surprising truths that could have a positive impact on your practice. In the first of two articles, Dean Pearson, NAB Head of Behavioural & Industry Economics and I explore the results and uncover similar thinking on holistic approaches to health and two very different attitudes to prevention.
The more you know about your patients’ attitudes and beliefs, the easier it is to build deeper relationships and provide more effective care. In turn, this can help you grow your business – but genuine feedback can be hard to find.
The 2019 NAB/Medfin Australian Consumer Health Survey was designed to bridge that knowledge gap by providing unique consumer insights. This year, around 1,000 Australians shared their views on their own health and how well they think the healthcare system can support them now and in the future.
The survey also gives practitioners a voice, with about 80 professionals taking part. By viewing health from both perspectives we were able to identify where patients and practitioners think along the same lines and, even more interestingly, where they don’t.
What does ‘healthy’ really mean?
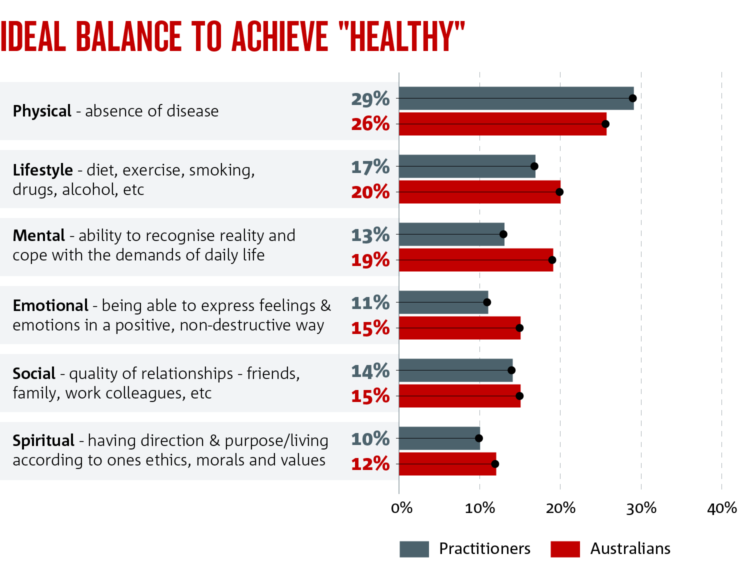
We looked first at what the word ‘healthy’ means to different people. Not surprisingly, the majority of practitioners and patients put the absence of disease first, but there’s also a strong indication that both groups are taking a more holistic view.
Lifestyle rated highly, and this was closely followed
by mental health and emotional wellbeing. In fact, more patients than practitioners thought that mental health and emotional wellbeing played an important role in their overall health.
How healthy do you think you are?
On average, patients considered themselves to be “reasonably” healthy across all measures, which included the absence of disease, lifestyle, quality of relationships, emotional health, purpose and mental health.
Almost three quarters of Australians over the age of 65 (72 per cent) have a condition requiring ongoing medical treatment or pharmaceutical support, so it follows that they ranked themselves lowest in terms of physical health. However, the fact that they rated highest for all other measures is consistent with the findings of NAB’s latest Wellbeing Survey (NAB Australian Wellbeing Report: Q2 2019) that, as we age, we tend to view many aspects of our non-physical wellbeing more favourably than younger people.
A particularly alarming statistic is that 34 per cent of people aged 18 to 24 identified as having a diagnosed mental health condition. It’s also a concern that those who rated themselves most in need of mental health services found them relatively prohibitive in terms of access and cost – particularly as 44 per cent of practitioners cited better follow-up for those with mental health problems as the initiative that would be most effective in preventing chronic problems.
Again, this reinforces NAB’s Wellbeing Survey, which found one in three Australians identify as having high levels of anxiety, and that anxiety is particularly prevalent in the 18 to 29 age group. Fewer practitioners than patients rated mental health as contributing to overall health (13 per cent vs. 19 per cent). However, when they were asked what initiatives they believe would be most effective in reducing levels of chronic health problems, 44 per cent of practitioners said better follow-up programs for those with mental health problems.
So, while the importance of mental health is being interpreted in slightly different ways, both patients are practitioners see a need for increased support.
Could chronic disease be prevented?
A large proportion of Australians (43 per cent) have an ongoing medical condition requiring treatment or medication. Clearly, the personal, social and economic impact of chronic illness on this scale constitutes a major challenge.
Practitioners believe that almost half of these conditions could be prevented through lifestyle, social, emotional or mental changes. However, in one of the most striking disconnects between practitioners and patients, only one in five patients believed prevention was possible through such means.
Over 65s are the least likely age group to acknowledge the power of prevention, while almost a third of those aged 18 to 24 are open to the idea. This shift in attitude in younger people could be critically important in the future. If it plays out as the adoption of relatively healthy behaviours, it could significantly reduce the societal incidence of chronic disease and its impact on the individual, as well as reduce expenditure around chronic disease very substantially. Unfortunately, as younger people actually rated their lifestyle the least healthy of all age groups, this may not eventuate.
Many practitioners favoured government action to reduce children’s exposure to junk food advertising and introduce a junk food tax. Practitioners would also encourage patients to take more responsibility for their health outcomes rather than relying on the system to make them healthy. This suggests there’s room for more education about the role of prevention.
Overall, NAB has a very positive view of the health sector and we see very strong opportunities for growth. There’s already increasing focus on patient experience as new technology provides consumers with unprecedented access to information, and forward-thinking practitioners are considering new business models to help meet consumers’ expectations for more personalised care.
In the second part of this series we’ll take a closer look at where some of these opportunities lie – the disconnect between what patients want and what practitioners assume they want.
Interested in reading more? Download the full 2019 NAB/Medfin Australian Consumer Health Survey
© National Australia Bank Limited. ABN 12 004 044 937 AFSL and Australian Credit Licence 230686.